Recent research provides evidence that Parkinson’s disease (PD) is associated with thinning of specific retinal layers that can be detected years before diagnosis.
Key facts:
- Individuals with Parkinson’s disease (PD) had thinner retinal ganglion cell and inner plexiform layers compared to controls.
- Thinning of the inner nuclear layer, which contains dopamine cells, was also seen in PD patients.
- Retinal thinning occurred years before PD diagnosis, suggesting it could aid early detection.
- Retinal changes may relate to neurodegeneration in the brain or primary retinal dopamine loss.
Source: Neurology 2023
Retinal Thinning Detected via OCT Before Parkinsons Onset
The study, published in JAMA Neurology, utilized two large cohort studies from the UK: (1) the AlzEye study of over 150,000 patients attending eye hospitals in London and (2) the UK Biobank prospective study of over 67,000 middle-aged adults.
Using optical coherence tomography (OCT) imaging of the retina, the researchers found thinner retinal ganglion cell-inner plexiform layer (GCIPL) and inner nuclear layer (INL) in people with prevalent PD compared to controls without PD.
Strikingly, those who went on to develop PD also had reduced GCIPL and INL thickness at baseline assessment on average 7 years prior to diagnosis.
These findings add weight to the potential for retinal imaging as a tool for early detection and monitoring of PD progression.
What the Retina Can Reveal About Parkinson’s Disease
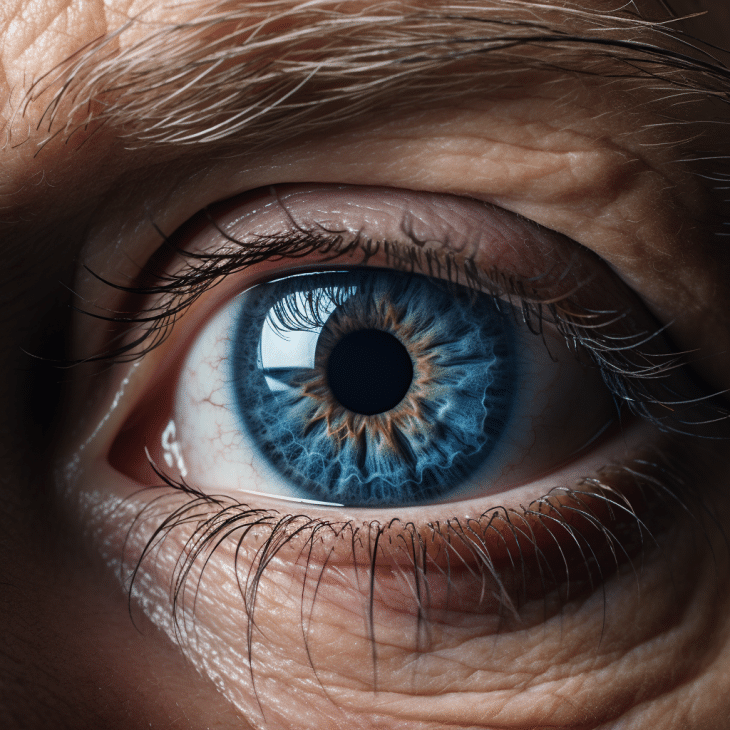
The retina offers a window into the central nervous system.
As an extension of the brain during embryonic development, it shares several features with brain tissue.
The inner nuclear layer of the retina harbors dopamine cells called amacrine cells, which constitute under 1% of retinal neurons yet are essential for visual processing.
Postmortem studies show dopamine deficiency and degeneration of amacrine cells in the retinas of PD patients.
Imaging modalities like OCT can measure thinning of the retinal layers in living individuals, reflecting neurodegeneration.
The ganglion cell layer contains cell bodies of retinal ganglion neurons that transmit visual information from photoreceptors to the brain.
The neighboring inner plexiform layer houses connections between retinal neurons.
As retinal manifestations of PD brain pathology, GCIPL thinning may occur through:
- Retrograde trans-synaptic degeneration from neurodegeneration in visual processing regions of the brain
- Anterograde degeneration from loss of retinal dopamine cells and their connections
Thinning of the INL points more specifically to pathology originating within the dopamine amacrine cells of the retina itself.
AlzEye & UK Biobank Studies: GCIPL & INL Thinning Detected
The AlzEye study included over 700 patients with prevalent PD identified from hospital records.
Compared to controls, PD patients showed significant GCIPL thinning (2.12 μm lower on average) and INL thinning (0.99 μm lower).
Effects were independent of potential confounders like age and diabetes.
In the UK Biobank cohort, GCIPL and INL thicknesses at baseline were associated with developing PD later on.
For each standard deviation higher thickness, the hazard ratio for future PD diagnosis was 0.62 for GCIPL and 0.70 for INL.
Importantly, retinal thinning preceded diagnosis by an average of 7 years.
While absolute differences in retinal thickness were small, they likely represent years of subtle neurodegeneration accumulating before PD symptoms appear and diagnosis is made.
The AlzEye findings demonstrate retinal changes are detectable at the prevalent disease stage using widely available OCT technology.
The UK Biobank results provide clues that similar retinal measurements could improve early diagnosis, but more research is needed.
Potential Significance for Parkinson’s Diagnosis and Prognosis
Current clinical diagnosis of PD relies mainly on presentation of motor symptoms, which manifest after 50-70% of dopamine neurons in the brain have already died.
At this late stage, many patients already have irreversible neurodegeneration.
Biomarkers that could detect PD pathology earlier would enable prognostic stratification and timely therapeutic interventions to slow progression.
Neuroimaging methods like dopamine transporter scanning can identify pre-motor PD, but availability is limited.
As the authors note, retinal OCT is low-cost, non-invasive, and widely accessible in clinics and even community optometry practices.
With further validation of its predictive value, retinal imaging could fill an important need for scalable PD screening and monitoring.
Future studies should explore whether patterns of retinal change mirror disease trajectories like speed of progression.
Retinal biomarkers could potentially track treatment responses and play a role in clinical trials.
Combining OCT with other diagnostics like blood or cerebral spinal fluid tests may provide a powerful precision medicine approach.
Mechanisms of Retinal Pathology – Brain vs Retina Origins?
While the AlzEye and UK Biobank studies clearly demonstrate retinal changes in PD, the underlying mechanisms require further study.
One possibility is that retinal thinning results from neurodegeneration in visual processing areas of the brain (e.g. lateral geniculate nucleus) via retrograde degeneration.
Alternatively, pathology could originate from loss of dopaminergic amacrine cells within the retina.
Longitudinal data on sequential changes in different retinal layers could help decipher the timeline and directionality of degeneration.
For instance, does INL thinning consistently precede GCIPL changes?
Combining retinal OCT with other neuroimaging modalities could also provide insight into brain versus retinal drivers of pathology.
Retinal dopamine deficiency and thinning of INL and GCIPL specifically in the parafoveal area implicate degeneration of amacrine cells and their connections as a contributor.
Immunostaining of postmortem PD retinas reveals loss of dopaminergic amacrine cells and abnormal morphology of linked ganglion cells.
While many questions remain, the collective evidence points to a possible primary retinal dopaminergic neuropathy that mirrors the brain pathology of PD.
Further research on the predictive value and progression of retinal biomarkers could open new doors for understanding PD pathogenesis and improving clinical care.
References
- Paper: Retinal Optical Coherence Tomography Features Associated with Incident and Prevalent Parkinson Disease (2023)
- Authors: Siegfried Karl Wagner et al.